Formthotics are custom-fitted medical orthotics, designed to provide support and comfort for your patients. A total contact foot orthotic – achieved by thermoforming (heat-moulding) the orthotic and fitting it to the patient’s foot. They form a vital part of our full-service medical system.





Formthotics Medical System
The Formthotics Medical System is a patient-centric process of assessment and management, utilising your expertise to quickly and effectively assess and treat your patient. This includes a comprehensive clinical method to improve lower limb function with custom-fitted Formthotics medical orthotics.

Formthotics medical range
Formthotics custom medical orthotics are only available to patients through their medical professional. With a unique design and manufacturing process, Foot Science International have created several distinguishing features that create the ultimate orthotic, in Formthotics. As a total contact foot orthotic, Formthotics provide the best possible neuromotor facilitation and biomechanical control, that naturally fit to your patients’ feet.
Custom-fitted | Thermoformable | Antimicrobial
Select the right Formthotics for your patient
Use our custom selection tool to help you identify the right product for your patient, their shoes, and their needs.
Heating
Custom Heat Moulding
Formthotics insoles are made from thermoformable foam, which means they mould to the foot and footwear of your patient and provide a custom solution.
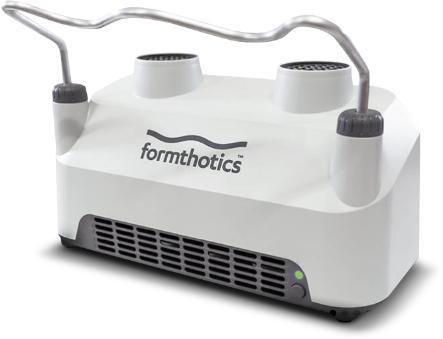
When the orthoses are in the patients’ shoes, they should be heated with the Formthotics V20 Heating Machine, specifically designed and tested to meet the highest standards of quality, functionality and results.
The Formthotics V20 Heating Machine heats the insoles to the optimum temperature for custom moulding. The patient can then wear their shoes instantly in-clinic. As the foam cools, the Formthotics set in the optimal position.